Diagnosing Anemia in Children
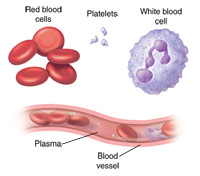
Anemia is a common condition in children. About 20% of children in the U.S. will be diagnosed with anemia at some point. A child who is anemic doesn't have enough red blood cells or enough hemoglobin. Hemoglobin is a special type of protein in red blood cells. It allows red blood cells to carry oxygen to other cells in the body.
Anemia has 3 main causes:
-
Loss of red blood cells from bleeding
-
Inability to make enough red blood cells
-
A medical condition that causes the destruction of red blood cells
Screening for anemia is an important part of caring for a child. Many problems caused by anemia can be prevented when anemia in children is diagnosed at an early stage. In most cases, anemia can be diagnosed with a few simple blood tests. The American Academy of Pediatrics currently advises screening for anemia with a hemoglobin test at age 1 year. It should include looking for risk factors for iron deficiency anemia. If the hemoglobin level is low, more testing is needed to find out the type of anemia. If a child has any risk factors at any age, a test for anemia should be done. For older children, a blood test for anemia may be done during a routine exam.
Symptoms of anemia in children
Many children with anemia have no symptoms. That's why it's important for children to have routine blood tests to check for the condition. Some of the signs and symptoms that might make a health care provider suspect anemia in a child include:
Blood tests for diagnosing anemia
To get a blood sample, a health care provider will insert a needle into a vein, usually in the child's arm or hand. A tourniquet may be wrapped around the child's arm to help the provider find a vein. Blood may be drawn up into a syringe or a test tube. In some cases, blood can be taken using a needle prick.
Blood tests may cause a little discomfort while the needle is inserted. The needle may cause some bruising or swelling. After the blood is withdrawn through the needle, the provider will remove the tourniquet. Then the needle is removed. The provider will put pressure on the area, and apply a bandage.
In most cases, a child won't need any special preparation or care after a blood test.
Most types of anemia in children can be diagnosed with these blood tests:
-
Hemoglobin and hematocrit. This is often the first screening test for anemia in children. It measures the amount of hemoglobin in the blood and the amount of red blood cells in the blood sample.
-
Complete blood count (CBC). If hemoglobin or hematocrit is abnormal, a complete blood count may be done. This test adds important information about the blood, including the size of red blood cells.
-
Peripheral smear. This test is done with a smear of blood on a slide that is checked under a microscope. By looking at a child's blood cells under a microscope, a lab specialist may be able to diagnose a type of anemia that causes red cells to grow or develop abnormally.
-
Reticulocyte count. Reticulocytes are immature blood cells. A reticulocyte count measures the amount of newly formed red blood cells in the child's blood sample. Anemia caused by not enough red blood cells being made results in a low reticulocyte count. Anemia caused by too many red blood cells being lost causes a high reticulocyte count.
Types of anemia in children
Children's anemia can be classified by the size of their red blood cells. The types are:
-
Microcytic anemia. This means the child's red blood cells are smaller than normal. The most common cause of microcytic anemia is iron deficiency.
-
Normocytic anemia. This means the child's red blood cells are normal in size. Normocytic anemia has many causes and may need other special types of blood tests.
-
Macrocytic anemia. This means the child's red blood cells are larger than normal. This is the rarest type of anemia in children. It may be caused by vitamin B 12 deficiency.
Treating anemia
Treating anemia in children depends on the type of anemia and its cause. In some cases, treatment may simply be a change in diet or the use of diet supplements. In other cases, a blood transfusion or long-term treatment may be needed.